Cataract Surgery and Treatment of Angle Closure Glaucoma
With age the crystalline lens behind the iris turns cloudy and thickens, pushing forward against the iris. If the patient’s anterior chamber (space between the iris and the cornea) is narrow to begin with, this pressure will eventually close off the anterior chamber, causing angle closure glaucoma.
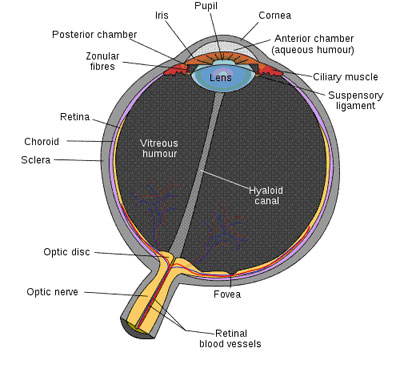
After cataract surgery the anterior chamber can increase in depth, lessening intraocular pressure. For patients with narrow anterior chambers, performing cataract surgery at an early stage can lessen complications associated with the procedure. As cataract surgery is carried out in the anterior chamber, depth is important. The more mature the cataract, the shallower the anterior chamber depth, increasing the risk of surgical injury to the endothelial cells. Endothelial cell damage eventually leads to corneal edema and degeneration. Also, with raised intraocular pressure, there is an increased risk of surgical difficulties and complications.
If the cornea and the iris stick together as the angle between them continues to narrow, this can cause permanent closure of the anterior chamber angle. It is best for cataract patients with angle closure glaucoma, or the likelihood of angle closure glaucoma, to get early cataract surgery.
Angle-closure glaucoma and cataracts are closely related. A maturing cataract can cause the onset and development of angle closure glaucoma. In addition, because of the narrow space in the anterior chamber and the high intraocular pressure, cataract surgery for angle closure glaucoma patients is more difficult and complication rates are higher.
Over the past 10-15 years, the success rate of cataract surgery has increased substantially. For patients with angle-closure glaucoma, early cataract removal can prevent, and in some cases cure, glaucoma.
